Coronary artery disease and what is management of coronory atery disease
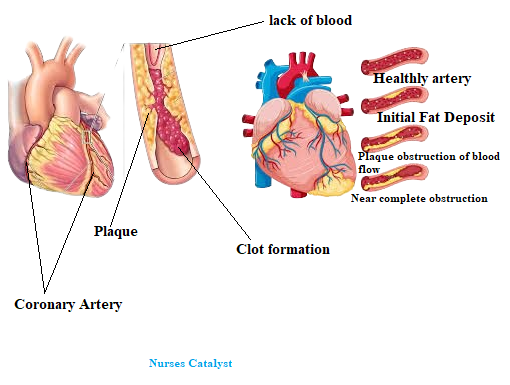
Coronary Artery Disease (CAD) happens when the arteries that supply oxygen-rich blood to the heart get blocked or narrowed. This can occur due to blood clots or fat buildup. Coronary artery disease leads to chest pain (angina), shortness of breath, heart attacks, and dizziness. To manage it, doctors often prescribe aspirin, angiotensin-converting enzyme inhibitors, and beta-blockers.
Coronary Artery Disease mainly happens when fat builds up in the coronary arteries. This buildup blocks or narrows the arteries. As a result, oxygen flow to the heart muscles decreases.
In this Article:
What is Coronary Artery Disease (CAD)?
CAD occurs when the coronary arteries narrow or block. These arteries supply oxygen-rich blood to your heart. The main cause is plaque buildup, which is a mix of fat, cholesterol, and other substances.
Risk factor for developing Coronary Artery Disease(CAD).
Modifiable Risk Factor( Risk factor that can be changed)
• High blood cholesterol (hyperlipidemia)
• Cigarette smoking, tobacco use
• Elevated blood pressure
• Hyperglycemia (diabetes mellitus)
• Metabolic syndrome
• Obesity
• Physical inactivity
Risk Factor that can Not Modifiable.
• Family history matters: a first-degree relative with heart disease at 55 or younger for men, and 65 or younger for women.
• Age "more than 45 years for men, more than 55 years for women".
• Gender "men develop cardiovascular disease at an earlier age than do women".
Sign and Symptoms of Coronary Artery Disease/Clinical Manifestations of CAD
Symptoms and complications depend on where fat builds up in the blood vessels. They also rely on how much fat is present, how narrow the arteries are, and if clots form. This can block blood flow to the heart muscle.
Symptoms include the following:
• Ischemia
• Chest pain: angina pectoris
• Atypical symptoms of myocardial ischemia "shortness of breath, nausea, and weakness"
• Myocardial infarction (MI)
• Dysrhythmias, sudden death
Medical Management Of Coronary Artery Disease/ Treatment of Coronary Artery Disease(CAD)
Treatment of Coronary Artery Disease it may refer to the treatment of Angina pectoris and Myocardial infraction.
Pharmacologic Therapy
• Nitrates, the mainstay of therapy "Nitroglycerin"
• Beta-adrenergic blockers "metoprolol and atenolol"
• Calcium channel blockers/calcium ion antagonists "amlodipine and diltiazem"
Antiplatelet and anticoagulant medications include:
Prevention
The main goal of management is to prevent high-density cholesterol. Four risk factors can be changed: cholesterol issues, tobacco use, high blood pressure, and diabetes.
Advice to the patient who has Coronary Artery Disease(CAD)
Follow a clear plan to manage the condition. This helps lower the risk of complications like heart attacks or strokes.
Medical management Advice.
Take Medications as Prescribed by physician
Common medication such as aspirin, beta-blockers, ACE inhibitors, or nitrates.
Don't skip doses — set reminders if needed.
Regular Check-ups
Follow up with your cardiologist regularly.
Check blood pressure, cholesterol, blood sugar (especially if diabetic).
Understand Your Condition
Learn about CAD, recognize symptoms of worsening "example, chest pain, shortness of breath", and when to seek emergency care.
Lifestyle advices
Heart-Healthy Diet
Focus on fruits, vegetables, whole grains, lean proteins (like fish, poultry), nuts, and healthy fats (olive oil, avocado).
Limit: salt, red meat, saturated fats, sugar, and processed foods.
Quit Smoking
If you smoke, seek help to quit. It's one of the most powerful changes you can make.
Limit Alcohol
If you drink, do so in moderation — the recommended amount is 1 drink per day for women and 2 drinks per day for men.
Stress Management Advices
Chronic stress can worsen CAD. Try:
Deep breathing
Meditation
Yoga
Counseling or therapy, if needed
Weight and Sleep Advices.
Maintain a healthy weight (BMI under 25).
Get 7–9 hours of quality sleep each night.
Treat conditions like sleep apnea if present.
Physical exercise Advices
Aim for at least 150 minutes of moderate aerobic activity each week. This can include activities like walking, swimming, or biking.
Add muscle-strengthening exercises twice a week.
Always consult your doctor before starting or modifying exercise routines