What are four Vital Sign and normal Range, what are management of an abnormal vital sign.
vital sign is the parameter of the health , it indicate how you body is functioning. or Indicators that permit to observe all changes in body or Indicators that permit to detect and monitor physiological changes and medical problems.
vital signs reflect changes that happen in our organism that otherwise might not be observed. vital signs are indicators of body functions . They are checked to monitor the functions of the body. All vital signs are objective data assessment that indicate how well or poorly the body is functioning.How many vital sign do we have?
we have 4Vital signs only :
- Temperature (T)
- Pulse (P)
- Respiration (R)
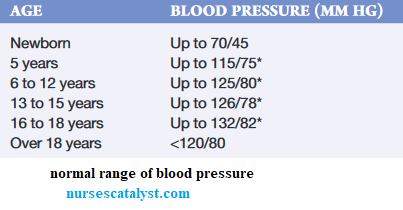
- Blood pressure (BP).
TPR-BP
Taking vital signs is to measure Temperature, Pulse, Respiration and Blood Pressure, oxygen saturation and pain assessment.
All vital signs are parameters but all parameters are not vital signs.
When to assess client’s vital signs?
- On patient admission to obtain baseline data
- On patient admission in hospitalization
- In case there is changes in the patient’s health status
- During physical examination
- Before and after administrating medications that could affect respiratory system, cardiovascular system and other systems
- Before and after surgery or invasive procedure
- Before and after nursing interventions that can affect vital signs
How often to assess client’s vital signs?
Chiefly, the frequency depends
1. On the client’s health status
2. Nursing judgement
3. Agency policy, hospital protocol
4. Physician orders
A. Temperature (T)
The body maintains a temperature range of between 35.8°C to 37.4 °C or from 96.6 °F to 99.3 °F, this being the optimum temperature range for the physiological functions of the body. This normal temperature range is maintained by keeping a balance between heat production and heat loss.
This continuous and unnoticed water is called insensible water loss and the accompanying heat loss is called insensible heat loss. The center for regulation of temperature is is located in the hypothalamus. The anterior hypothalamus promote heat loss and The posterior hypothalamus promote heat production and heat conservation.
Conversion of temperature scales
To convert from Fahrenheit to Celsius °C = (Fahrenheit temperature – 32) x 5/9
To convert from Celsius to Fahrenheit °F = (Celsius temperature x 9/5) + 32
Purposes of taking or measuring body temperature.
- To establish baseline data for subsequent evaluation
- To identify whether the core temperature is within normal range
- To determine changes in the core temperature in response to therapies i.e. treatments
- To monitor clients at risk for imbalanced body temperature
Types of thermometer
- Mercury-in-glass thermometers
- Electronic thermometers (Digital)
- Infrared thermometer
- Temporal artery thermometer
- Temperature-sensitive tape
- Chemical disposable thermometers.
Sites for body temperature measurement
Temperature is commonly measured in 3 sites
- Oral
- Axillary
- Rectal
Other sites are
- Tympanic membrane
- Skin
- Temporal artery
1. Oral Temperature
Indications: conscious adult , Wasted patient (cachectic)
Contraindications:
- hot and cold drinks intake or after smoking
- Unable to close the mouth
- Obstacle: infection or intervention of the mouth
- Infants and children under six
- Confused or comatose patients
- Convulsions
- Patients suffering from nausea or vomiting
- Patients under oxygen by a mask
2. Axillary temperature
Taking the temperature by axilla measures the surface temperature of the body, and this method is not accurate if not correctly carried out.
Indications: Conscious adult, Functional arm, newborns
Contraindications: small children, Unconscious patient, Agitated patient
Advantages: Safest and least invasive method, Less potential for spreading microorganisms with than the oral and rectal
Disadvantage: Breaking of material (thermometer), requires the longest time for assessment of 5 minutes or longer
3. Rectal temperature
The rectal temperature is considered to be the most accurate method of taking the temperature, and it is a true reflection of the core temperature of the body.
Indications :Infants, Unconscious patient, Every time that some doubts exist on a febrile state
Contra-indications : Diarrhea, Affection or anal injury, Rectal surgery
Advantages : More reliable measurement
Disadvantages : Injury to the rectum is possible, More unpleasant for clients, difficult for clients who cannot turn to the side, presence of stool may interfere thermometer placement.
Surface temperature generally ranges from 35.8°C to 37.4 °C or from 96.6 °F to 99.3 °F
Normal Range for Adult:
Orally 36,7oC to 37,2o C
Axillary 35,6oC to 36,7o C
Rectally 36,7oC to 37,8o C
New born 36.1- 37.7 (axillary)
Alterations in body temperature
2 primary alterations:
Pyrexia and Hypothermia
Pyrexia also called Hyperthermia : body temperature above the normal range (High temperature).
Hypothermia: body temperature below the lower limit of normal (Low temperature).
Pyrexia or Hyperthermia or Fever(general term) : a body temperature above the usual normal range (generally T > 38 °C, 100.4 °F)
- A client with fever is referred to as febrile
- A client who does not have fever is afebrile
- A very high level of fever is called Hyperpyrexia
Hyperpyrexia : this is a state of hyperthermia characterized by an intense febrile state. Elevation of the temperature to 41 °C
( 105.8 °F)and beyond.
Heat exhaustion
An increase in body temperature (38°- 40°C; 100.4°- 104.0°F) in response to environmental conditions that, in turn, causes diaphoresis (profuse perspiration).
It is characterized by Loss of excessive amounts of water and sodium from perspiring leads to thirst, nausea, vomiting, weakness, fainting and disorientation.
A critical increase in body temperature (41°–44°C) resulting from exposure to high environmental temperatures
Dry, hot skin is the most important sign.
The person becomes confused, or delirious, and experiences thirst, abdominal distress, muscle cramps, and visual disturbances. Loss of consciousness occurs if untreated.
There is 4 common types:
- Intermittent fever
- Remittent
- Relapsing
- Constant
Remittent fever A wide range of temperature fluctuations (more than 2 °C) occurs over 24-hour period, all of which are normal. for example fever due to influenza.
Relapsing fever Short febrile periods of few days are interspersed with period of 1 to 2 days of normal temperature for example Tuberculosis fever.
Constant fever Body temperature fluctuates minimally but always remains above normal. for example Typhoid fever.
The clinical signs of fever vary with the onset, course and abatement stages of the fever.
Clinical manifestations of fever
Onset (cold or chill stage)
- Increased heart rate, Increased respiratory rate
- Shivering due to increased skeletal muscle tension and contractions
- Pallid, cold skin due to vasoconstriction
- Cyanotic nail beds due to vasoconstriction
- Complaints of feeling cold
- “Gooseflesh” appearance of the skin due to contraction of the arrectores pilorum muscles
- Cessation of sweating
- Rise in body temperature
Nursing intervention related to the fever
1. Monitor vital signs
2. Remove the client from the cold and rewarming the client’s body
3. Remove any wet clothes which exacerbate heat loss
4. Provide dry clothing
5. Apply warm blankets (cover the client with warm blanket)
6. Keep limbs close to body
7. Provide warm oral fluids (if the victim is conscious)
8. Warm the patient’s bed with heat pack
9. In case of aggravation, warmed intravenous fluids are given
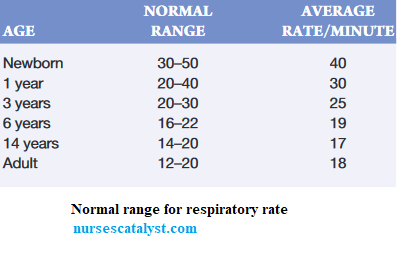
Respiration is the act of breathing, it includes the intake of oxygen and the output of carbon dioxide. The mechanical phenomena that rule the respiration appear in two times: the inspiration and the expiration
1. Inspiration (inhalation) is the intake of air into the lungs
2. Expiration (exhalation) is the movement of gases from the lungs to the atmosphere or breathing out.
Respiration is defined by physiological functioning as:
External respiration is the exchange of oxygen and carbon dioxide between the alveoli of the lungs and the pulmonary blood system
Internal respiration is the interchange of oxygen and carbon dioxide between the circulating blood and cells throughout the body.
Ventilation is word that is used to refer to the movement of air in and out of the lungs Or the inflow and outflow of air between the atmosphere and the lung alveoli.
Vital capacity is the amount of air exhaled from the lungs after a minimal full inspiration.
Hyperventilation refers to very deep, rapid respirations
Hypoventilation refers to very shallow respirations.
Deep respirations are those in which a large volume of air is inhaled and exhaled, inflating most of the lungs.
Shallow respirations involve the exchange of a small volume of air and often the minimal use of lung tissue.
They are basically two types of breathing that nurses observe, costal (thoracic) breathing and abdominal (diaphragmatic) breathing.
Characteristics of respiration
A normal breathing doesn't ask for any effort.
Respiration is characterized by:
1. Frequency (Rate) : this is the number of the movements expressed in minute
2. Rhythm : regular or irregular this is the succession to regular intervals of the inspiration and the expiration.
3. Amplitude : the amplifications more or less accentuated of the rib cage
4. Sound : Normally the breathing is inaudible
Respiration Rate per minute According to Age
Pulse and Blood Pressure
The Pulse and Blood pressure are physiological manifestations of circulatory system, constituted by the heart, vessels, (arteries, veins and capillaries) and blood.
Pulse
The pulse is the bounding of blood flow in an artery that is palpable at various points on the body The pulse is caused by the stroke volume ejection and distension of the walls of the aorta, which creates a pulse wave as it travels rapidly toward the distal ends of the arteries. As the pulse wave reaches a superficial peripheral artery and travels over an underlying bone or muscle, the pulse can be palpated by applying gentle pressure over a pulse point. Pulse is the rhythmic beating of the arteries due to the passage of blood propelled by every cardiac contraction. It is a wave of blood created by contraction of the left ventricle of the heart. It informs us on heart activities and on its rhythm.
Cardiac rhythm: Succession of contractions and relaxations that allows the heart to accomplish its function of pumping at a regular rhythm.
A peripheral pulse: is a pulse located in the periphery of the body, for example , in the foot, hand, or neck
Apical pulse, in contrast, is a central pulse; that is located at the apex of the heart
Features of pulse
A. Frequency.
Pulse is expressed in heart beatings per minute. It is the number of beatings of an artery discerned by the finger in determined time (usually during one minute).
Normal values of pulse per age:
Age Normal heart rate (beats per minute)
Foetus 120-160
Newborn 100-170
1 year 100-120
2-5 years 80-100
6–10 years 70-110
Adult 60-100
Old people 60-70
B. Rhythm:
Succession to equal interval of equal amplitude beatings.
A normal pulse is characterized by the regularity of beatings. Normally, the cardiac rhythm is regular, even in physiological factors.
An irregular pulse is a pulse that presents an
irregular rhythm.
Volume and amplitude: Indicate the power of the beatings.
C. Volume:
Volume is the importance of the blood flux that not only depends on the strength of the cardiac systole, but also of the elasticity of the arteries.
D. Amplitude:
Amplitude is the intensity of pulsation, that is depended on resistance strength and blood pressure, it is normally the same at every beating.
Tension or resistance: This is the strength that the pulse resists the compression of the finger on the artery when taking the pulse.
Factors that influence the cardiac rhythm (pulse rate) include:
1. Age
2. Sex
3. Activity – exercise
4. Emotion
5. Fever
6. Digestion
7. Medications
8. Bleeding (Hemorrhage)
Pulse abnormalities
Frequency: Tachycardia and Bradycardia
a) Tachycardia or accelerated pulse
1. Excessive cardiac frequency, high to the normal, (more than 100 beats per minute) for adult. It can reach 120 to 160 beatings per minutes and even more.
2. We say tachycardia when the rhythm remained regular
3. We say tachyarrhythmia when it is fast and irregular.
b) Bradycardia (low pulse rate)
1. Low heartbeat rate (less than 60 beatings per
minute for an adult person).
2. We say bradycardia when the rhythm remains
regular and of bradyarrhythmia when it is slow and
irregular.
Rhythm
1. Dysrhythmia or arrhythmia: a pulse with an
irregular rhythm. Tension or resistance disorders
In case of high blood pressure, the pulse gives the impression of a hard, rigid thread that rolls under the finger
2 TYPES OF PULSE
Dicrotic pulse: Perception of two heartbeats for one diastole: the finger discerns a very strong beating and a weak beating, only count the strong beatings
Bisferiens pulse: Perception of two heartbeats for one systole: the finger discerns a very strong beating and a weak beating, only count the strong beatings.
Pulse is assessed in different sites, the common sites are:
1. Radial artery; This is the most commonly used. It is easily found in most people. Radial artery passes along the radial bone, on the thumb side of the inner aspect of the wrist.
2. Brachial artery : pass in antecubital fossa
3. Temporal artery (over the temporal bone of the head)
4. Carotid artery (at the side of the neck below the lobe of the ear).
5. Femoral artery: where the femoral artery passes
alongside the inguinal ligament
6. Popliteal artery: where the popliteal artery passes
behind the knee
7. Posterior tibial artery: on the medial surface of the
ankle where the posterior tibial artery passes behind
the medial malleolus
8. Pedal (dorsalis pedis): where the dorsalis pedis artery passes over the bones of the foot
Precaution
1. The pulse is taken on a patient at rest, sitting or lying down.
2. Do not use thumb or just one or two fingers but always 3 fingers to feel the pulse.
3. Do not press the artery with more force.
Materials are Watch with second hand, Red pen and graphic chart, Stethoscope if apical pulse is to be taken
BLOOD PRESSURE
Blood pressure is the measurement of pressure pulsations exerted against the blood vessel walls during systole and diastole.
The cardiovascular system is a closed system and the measure of blood pressure determines the pressure of blood inside this system.
It is measured in terms of millimeters of mercury (mm Hg) as standard But this can be converted to centimeters (cmHg)
The blood pressure gives two measures respondent to the cardiac contraction:
The maximum (Maxima) indicates the measure of the systolic pressure, and the minimum (Minima) indicates the measure of diastolic pressure.
The variation of those two measures is the indication of assessment of cardiac activities and resistance offered by peripheral vessels.
The systolic blood pressure
Systolic pressure is the pressure exercised by the blood flow on the arterial wall at the time of the systole.
The diastolic blood pressure
It is the pressure exercised by blood on the arteries during the diastole. This minimum pressure is constant on the level of the arteries.
Pulse pressure: