Drugs For Fluids, Electrolytes And Acid-base Balance and Why is important to maintain it balance?
Fluid Therapy
The volume and composition of fluids in the body must be maintained within narrow limits. Excess fluid volume can lead to hypertension, congestive heart failure, or peripheral edema, whereas depletion results in dehydration and perhaps shock. Body fluids must also contain specific amounts of essential ions or electrolytes and be maintained at particular pH values. Accumulation of excess acids or bases can change the pH of body fluids and rapidly result in death if left untreated.
This chapter examines drugs used to reverse fluid balance, electrolyte, or acid–base disorders.
Fluids Balance and Body Fluids Compartment
Body fluids travel between compartments, which are separated by semipermeable membranes. Control of water balance in the various compartments is essential to homeostasis. Fluid imbalances are frequent indications for pharmacotherapy. The greatest bulk of body fluid consists of water, which serves as the universal solvent in which most nutrients, electrolytes, and minerals are dissolved. Water alone is responsible for about 60% of the total body weight in a middle-age adult. A newborn may contain 80% water, whereas an older adult may contain only 40%.
In a simple model, water in the body can be located in one of two places, or compartments: Intracellular and extracellular
1. The intracellular fluid (ICF) compartment: which contains water that is inside cells, accounts for about two thirds of the total body water(2/3TBW)
The remaining one third of body fluid resides outside cells in the extracellular fluid (ECF) compartment. The ECF compartment is further divided into two parts: fluid in the plasma, or intravascular space, and fluid in the interstitial spaces between cells.
There is a continuous exchange and mixing of fluids between the various compartments, which are separated by membranes: the plasma membranes of cells separate the ICF from the ECF. The capillary membranes separate plasma from the interstitial fluid. Although, water travels freely among the compartments, the movement of large molecules and those with electrical charges is governed by processes of diffusion and active transport. Movement of ions and drugs across membranes is a primary concept of pharmacokinetics
Osmolality, Tonicity and Movement of body fluids.
Osmolality and tonicity are two related terms central to understanding fluid balance in the body. Large changes in the osmolality or tonicity of a body fluid can cause significant shifts in water balance between compartments. Nurses will often administer intravenous (IV) fluids to compensate for these changes.
The osmolality of a fluid is a measure of the number of dissolved particles, or solutes, in 1 kg (1 L) of water. In most body fluids, three solutes determine the osmolality include sodium, glucose, and urea. Sodium is the greatest contributor to osmolality due to its abundance in most body fluids. The normal osmolality of body fluids ranges from 275 to 295 milliosmols per kilogram (mOsm/kg).
The term tonicity is sometimes used interchangeably with osmolality, although they are slightly different. Tonicity is the ability of a solution to cause a change in water movement across a membrane due to osmotic forces. Whereas, osmolality is a laboratory value that can be precisely measured, tonicity is a general term used to describe the relative concentration of IV fluids.
The tonicity of the plasma is used as the reference point when administering IV solutions
- Normal plasma is considered isotonic: Solutions that are isotonic have the same concentration of solutes (same osmolality) as plasma.
- Hypertonic solutions contain a greater concentration of solutes than plasma,
- Hypotonic solutions have a lesser concentration of solutes than plasma.
Through osmosis, water moves from areas of low solute concentration (low osmolality) to areas of high solute concentration (high osmolality).
If a hypertonic (hyperosmolar) IV solution is administered, the plasma gains more solutes than the interstitial fluid. Water will move, by osmosis, from the interstitial fluid compartment to the plasma compartment. This type of fluid shift removes water from cells and can result in dehydration Water will move in the opposite direction, from plasma to interstitial fluid, if a hypotonic solution is administered. This type of fluid shift could result in hypotension due to movement of water out of the vascular system. Isotonic solutions will produce no net fluid shift.
Thing You have to Know.
- Isotonic solution: Normal plasma volume because there is equal osmolarity and no net fluid change.
- Hypertonic solution: expand plasma volume due to increased osmolality in plasma, Water moves from cells and interstitial fluid to plasm
- Hypotonic solution: decreased plasma volume due to decreased osmolality in plasma, Water moves from plasma to interstitial fluid and cells
Regulation of fluid intake and Output
The average adult has a water intake of approximately 2,500 mL/day, most of which comes from ingested food and beverages. Water output is achieved through the kidneys, lungs, skin, feces, and sweat. To maintain water balance, water intake must equal water output. Net gains or losses of water can be estimated by changes in total body weight.
The most important physiological regulator of fluid intake is the thirst mechanism:
- The sensation of thirst occurs when osmoreceptors in the hypothalamus sense that the ECF has become hypertonic.
- Saliva secretion diminishes and the mouth dries, driving the individual to drink liquids. As the ingested water is absorbed, the osmolality of the ECF falls and the thirst center in the hypothalamus is no longer stimulated.
The kidneys are the primary regulators of fluid output.
- Through activation of the renin–angiotensin–aldosterone system, the hormone aldosterone is secreted by the adrenal cortex. Aldosterone causes the kidneys to retain additional sodium and water in the body, thus increasing the osmolality of the ECF.
- A second hormone, antidiuretic hormone (ADH), is released by the pituitary gland during periods of high plasma osmolality. ADH acts directly on the distal tubules of the kidney to increase water reabsorption. This increased water in the intravascular space dilutes the plasma, thus lowering its osmolality Failure to maintain proper balance between intake and output can result in fluid balance disorders that are indications for pharmacologic intervention.
Fluid deficit disorders can cause dehydration or shock, which are treated by administering oral or IV fluids. Fluid excess disorders are treated with diuretics . In the treatment of fluid imbalances, the ultimate goal is to diagnose and correct the cause of the disorder while administering supporting fluids and medications to stabilize the patient.
Fluid Replacement Agents with Cristaloids &Colloids
- Net loss of fluids from the body can result in dehydration and shock. IV fluid therapy is used to maintain blood volume and support blood pressure.When fluid output exceeds fluid intake, volume deficits may result. Shock, dehydration, or electrolyte loss may occur; large deficits are fatal, unless treated.The following are some common reasons for fluid depletion:
- Loss of gastrointestinal (GI) fluids due to vomiting, diarrhea, chronic laxative use, or GI suctioning.
- Excessive sweating during hot weather, athletic activity, or prolonged fever.
- Severe burns.
- Hemorrhage.
- Excessive diuresis due to diuretic therapy or uncontrolled diabetic ketoacidosis
Goal of fluids therapy
1. The immediate goal in treating a volume deficit disorder is to replace the depleted fluid.
1. In non acute circumstances, this may be achieved by drinking more liquids or by administering fluids via a feeding tube, whereas in acute situations, IV fluid therapy is indicated.
3. Regardless of the route, careful attention must be paid to restoring normal levels of blood elements and electrolytes as well as fluid volume.
4. IV replacement fluids are of two basic types: crystalloids and colloids
Comparison between colloid and crystalloids
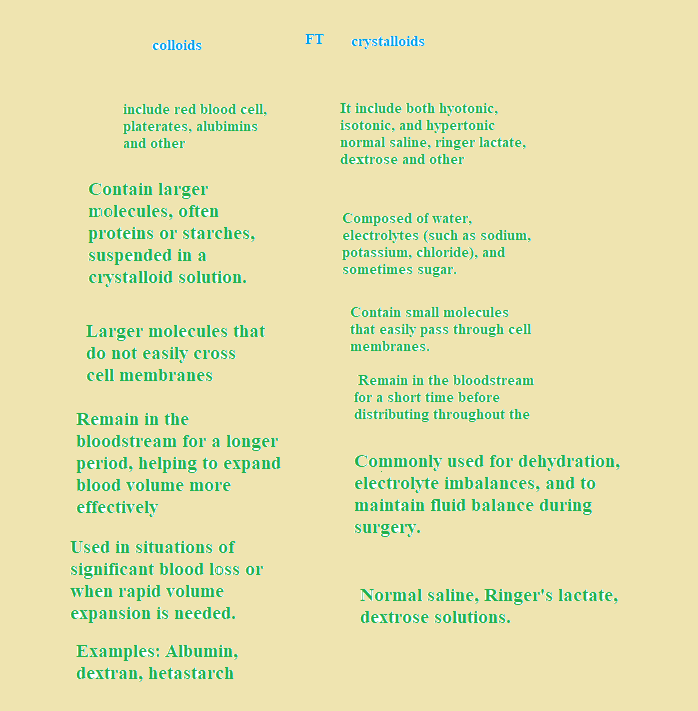
Crystalloids drugs/Fluids
Crystalloids are IV solutions that contain electrolytes and other substances that closely mimic the body’s ECF. They are used to replace depleted fluids and to promote urine output. Crystalloid solutions are capable of quickly diffusing across membranes, leaving the plasma and entering the interstitial fluid and ICF. It is estimated that two thirds of infused crystalloids will distribute in the interstitial space. Isotonic, hypotonic, and hypertonic solutions are available. Sodium is the most common crystalloid added to solutions.
Some crystalloids contain dextrose, a form of glucose, commonly in concentrations of 2.5%, 5%, or 10%.
Dextrose is added to provide nutritional value: 1 L of 5% dextrose supplies 170 calories. In addition, water is formed during the metabolism of dextrose, enhancing the rehydration of the patient. When dextrose is infused, it is metabolized, and the solution becomes hypotonic. Infusion of crystalloids will increase total fluid volume in the body, but the compartment that is most expanded depends on the solute (sodium) concentration of the fluid administered:
Isotonic crystalloids :can expand the circulating intravascular (plasma) fluid volume without causing major fluid shifts between compartments Isotonic crystalloids such as normal saline are often used to treat fluid loss due to vomiting, diarrhea, or surgical procedures, especially when the blood pressure is low. Because isotonic crystalloids can rapidly expand circulating blood volume, care must be taken not to cause fluid overload in the patient.
Infusion of hypertonic crystalloids: expands plasma volume by drawing water away from the cells and tissue These agents are used to relieve cellular edema, especially cerebral edema. When patients are dehydrated and have hypertonic plasma, a solution that is initially hypertonic may be infused, such as D5 0.45% NS, that matches the tonicity of the plasma. This allows the fluid to enter the vascular compartment without causing a net fluid loss or gain in the cells. As the dextrose is subsequently metabolized, the solution becomes hypotonic. This hypotonic solution then causes water to shift into the intracellular space, relieving the dehydration within the cells. A solution of 3% normal saline is hypertonic and usually reserved for treating severe hyponatremia.
Overtreatment with hypertonic crystalloids such as 3% normal saline can lead to excessive expansion of the intravascular (plasma) compartment, fluid overload, and hypertension.
Hypotonic crystalloids :will cause water to move out of the plasma to the tissues and cells in the intracellular compartment; thus, these solutions are not considered efficient plasma volume expanders. Hypotonic crystalloids are indicated for patients with hypernatremia and cellular dehydration.
Care must be taken not to cause depletion of the intravascular compartment (hypotension) or too much expansion of the intracellular compartment (peripheral edema).
Patients who are dehydrated with low blood pressure should be given normal saline; patients who are dehydrated with normal blood pressure should be given a hypotonic solution.
Colloids fluids
Colloids are proteins, starches, or other large molecules that remain in the blood for a long time because they are too large to easily cross the capillary membranes. While circulating, they have the same effect as hypertonic solutions, drawing water molecules from the cells and tissues into the plasma through their ability to increase plasma osmolality and osmotic pressure. Sometimes called plasma volume expanders, these solutions are particularly important in treating hypovolemic shock due to burns, hemorrhage, or surgery.
The most commonly used colloid is normal serum albumin, which is featured as a prototype drug for shock. Several colloid products contain dextran, a synthetic polysaccharide. Dextran infusions can double the plasma volume within a few minutes, although its effects last only about 12 hours. Plasma protein fraction is a natural volume expander that contains 83% albumin and 17% plasma globulins. Plasma protein fraction and albumin are also indicated in patients with hypoproteinemia. Hetastarch is a synthetic colloid with properties similar to those of 5% albumin, but with an extended duration of action.
Electrolytes: Physiological and Roles
Electrolytes are small charged molecules essential to homeostasis. Too little or too much of an electrolyte can result in serious complications and must be quickly corrected. Minerals are inorganic substances needed in very small amounts to maintain homeostasis. Minerals are held together by ionic bonds and dissociate or ionize when placed in water.
The resulting ions have positive or negative charges and are able to conduct electricity, hence the name electrolyte. Positively charged electrolytes are called cations; those with a negative charge are anions. Electrolyte levels are measured in units of milliequivalents per liter (mEq/L).
PHYSIOLOGY AND ROLES
Electrolytes are essential to many body functions including
- nerve conduction
- membrane permeability
- muscle contraction
- water balance
- bone growth and remodeling
Levels of electrolytes in body fluids are maintained within very narrow ranges, primarily by the kidneys and GI tract. As electrolytes are lost due to normal excretory functions, they must be replaced by adequate intake; otherwise, electrolyte imbalances will result. Although imbalances can occur with any ion, Na+ , K+ , and Ca2+ are of greatest importance.
An electrolyte imbalance is a sign of an underlying medical condition that needs attention: Imbalances are associated with a large number of disorders, with renal impairment being the most common cause. In some cases, drug therapy itself can cause the electrolyte imbalance. For example, aggressive therapy with loop diuretics such as furosemide (Lasix) can rapidly deplete the body of sodium and potassium.
Goal for Electrolytes & minerals therapy
The therapeutic goal is to quickly correct the electrolyte imbalance while the underlying condition is being diagnosed and treated. Treatments for electrolyte imbalances depend on the severity of the condition and range from simple adjustments in dietary intake to rapid electrolyte infusions. Serum electrolyte levels must be carefully monitored during therapy to prevent imbalances in the opposite direction; levels can change rapidly from hypo-concentrations to hyper-concentrations.
Pharmacotherapy of Sodium imbalances
Sodium ion (Na+ ) is the most abundant cation in extracellular fluid. Because of sodium’s central roles in neuromuscular physiology, acid–base balance, and overall fluid distribution, sodium imbalances can have serious consequences. Although definite sodium monitors or sensors have yet to be discovered in the body, the regulation of sodium balance is well understood. Sodium balance and water balance are intimately connected. As Na+ levels increase in a body fluid, solute particles accumulate, and the osmolality increases. Water will move toward this area of relatively high osmolality. In simplest terms, water travels toward or with Na+ . The physiological consequences of this relationship cannot be overstated.
Pharmacotherapy of anaphylaxis.
Anaphylaxis is a potentially fatal condition in which body defenses produce a hyper response to a foreign substance known as an antigen or allergen. On first exposure, the allergen produces no symptom but the body responds by becoming highly sensitized for a subsequent exposure. The body responds quickly, often just minutes after exposure to the allergen, by releasing massive amounts of histamine and other inflammatory mediators. The patient may experience itching, rashes, and a tightness in the throat or chest.
Swelling occurs around the larynx, causing a nonproductive cough and the voice to become hoarse.
As anaphylaxis progresses, the patient experiences a rapid fall in BP and difficulty breathing due to bronchoconstriction. The hypotension causes reflex tachycardia. Without medical intervention, anaphylaxis leads to a profound state of shock, which is often fatal.
Clinically patient will present the following signs on
1. Heart: fast heart rate with and decreased cardiac output
2. Arterioles: generalized vasodilation and edema
3. Lungs: bronchoconstriction with expiratory dyspnea
4. Skin: Itching and generalized rashes
Pharmacotherapy management
The pharmacotherapy of anaphylaxis is symptomatic and involves supporting the cardiovascular system and preventing further hyper response by body defenses. Various medications are used to treat the symptoms of anaphylaxis, depending on the severity of the symptoms .
The following actions must be initiated immediately:
1.Epinephrine: 1:1000 given subcutaneously or intramuscularly (IM), is an initial drug of choice because it causes vasoconstriction and can rapidly relieve symptoms of bronchoconstriction .If necessary, the dose may be repeated up to three times at 10- to 15-minute intervals.
2. Crystalloids or colloids may be needed to prevent shock if the patient presents with volume depletion.
3. Antihistamines such as diphenhydramine (Benadryl) may be administered IM or IV to prevent further release of histamine
4.A bronchodilator such as albuterol (Proventil, Ventolin, VoSpire) is often administered by inhalation to relieve the acute shortness of breath caused by histamine release.
5. High-flow oxygen is usually administered to maintain oxygenation
6.Systemic corticosteroids such as hydrocortisone are given to inhibit the delayed inflammatory response that may occur several hours after the initial event
Practically all drugs have the capability to cause anaphylaxis but this is a rare adverse drug effect, nurse must be prepared to quickly deal with anaphylaxis by understanding the indications and doses of the various drugs on the emergency cart
Common drugs causing
The most common drugs causing anaphylaxis include the following:
1. Antibiotics, especially penicillin, cephalosporins, and sulfonamides.
2.Nonsteroidal anti-inflammatory drugs (NSAIDs), such as aspirin, ibuprofen, and naproxen.
3.Angiotensin-converting enzyme (ACE) inhibitors.
4.Opioid analgesics.
5.Iodine-based contrast media used for radiographic exams.
PREVENTION
1.Effetive history taking: obtaining a patient history of drug allergy is helpful in predicting some adverse drug reactions but anaphylaxis may occur without a previously reported incident. However, previous severe hypersensitivity to a drug is always a contraindication to the future use of that or closely related drugs in the same class. Unless the drug is the only one available to treat the patient’s condition, it should not be administered
2. Immunosuppression agents : If a drug must be given for which the patient has a known allergy, the patient may be pretreated with antihistamines or glucocorticoids to suppress the inflammatory response.
3.Desensitization:If time permits, patients may be desensitized. Desensitization for penicillin and cephalosporin allergy, which takes about 6 hours, has been shown to be effective in preventing severe allergic reactions to these antibiotics. A typical desensitization regimen would involve administering an initial dose of 0.01 mg of the antibiotic and observing the patient for allergy. The dose may then be doubled every 15 to 20 minutes until the full dose has been achieved. Desensitization has also been achieved for patients with aspirin-induced asthma who require aspirin therapy for another condition.